New Technique Isolates Brain Cells Associated With Parkinson's Disease Analysis Shows Changes in How Diseased Cells Sense and Use Oxygen
Byron SpiceThursday, November 19, 2020Print this page.
Carnegie Mellon University researchers have developed a new technique for isolating a type of brain cell associated with Parkinson's disease symptoms, enabling them to study that cell type in detail.
The technique, which works only in specially bred mice, costs less than previous methods for isolating these brain cells, said Alyssa Lawler, a Ph.D. student in biological sciences. By using it, she and her colleagues already have detected previously undiscovered changes to how the diseased neurons sense and use oxygen.
The researchers describe the technique and their findings in a research paper published online by the journal JNeurosci.
"Even a small portion of the brain can have dozens of different cell types," said Andreas Pfenning, an assistant professor in CMU's Computational Biology Department. "Each of these cell types has different roles in the behavior of an animal and also in disease." Separating cells of a certain type from their neighbors is thus a critical first step for researchers who want to study them.
In this case, the research team focused on parvalbumin-expressing (PV+) neurons, which have been implicated in Parkinson's disease by the lab of Aryn Gittis, associate professor of biological sciences. Mice with Parkinson's symptoms regain motor control and their ability to run around when these cells are stimulated.
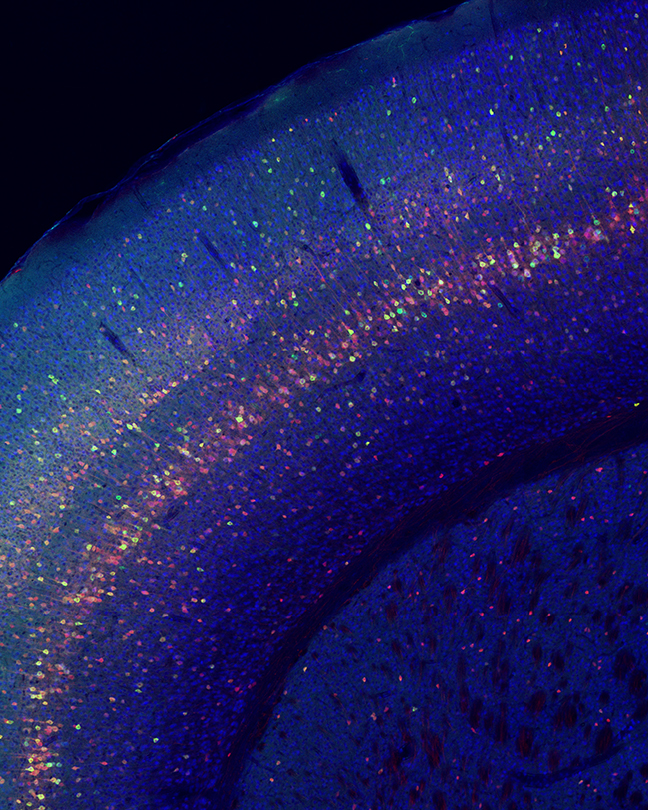
Lab mice have been bred with PV+ cells that contain a protein called Cre that activates a fluorescent green protein. That fluorescence makes it possible for cell-sorting machines to isolate the cells from others in a mixture. But cell-sorting machines are extremely expensive, so Lawler developed a cheaper method, called Cre-Specific Nuclear Anchored Independent Labeling, or cSNAIL.
The new technique uses a virus commonly employed by researchers to deliver DNA to brain cells. When the virus enters PV+ cells, Cre causes the tag to fluoresce. In the case of cSNAIL, researchers use antibodies to detect the tag and pull the PV+ nuclei away from other cells.
"The technique turned out to be really specific, really efficient," Lawler said, noting that it can be adapted to other mouse models that use the Cre protein.
In a subsequent analysis of the PV+ neurons, the researchers found that those from sick mice produced more RNA involved in the expression of genes that sense or use oxygen. Further study also showed that the DNA in the nucleus unwound in ways indicating that the oxygen-sensing genes were more active.
"Oxygen-sensing pathways have been implicated in other, earlier aspects of Parkinson's disease, but not previously in PV+ cells," Lawler said. These pathways are involved in both protecting and killing cells during neurodegeneration.
Pfenning noted that datasets from this study are part of a larger effort to build machine learning models that will help researchers interpret disease mechanisms by looking at how particular DNA sequences respond to different conditions across types of cells.
"We're learning how to talk to cells, to speak their language," Lawler said.
The National Institutes of Health and the National Science Foundation supported this research.
Byron Spice | 412-268-9068 | bspice@cs.cmu.edu
